Fungal Acne
fuhng · gl -ak · neeFungal acne isn’t acne at all—but it certainly looks like it. Similar pimple-like bumps appear, but the cause is a fungal infection that requires a totally different treatment than acne does.
Also Called
Pityrosporum folliculitis, malassezia folliculitis
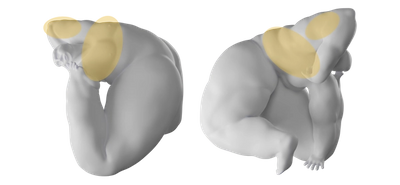
Frequently Found On
Chest, back, and arms
What is fungal acne?
If you’ve been attacking a recent breakout of acne with everything in your arsenal—cleansers, spot treatments, exfoliators, salicylic acid for days, even those little pimple patches—and it won’t quit, it might be a case of fungal acne. Confusingly, fungal acne isn’t actually acne at all, but a fungal infection called pityrosporum folliculitis that just looks like acne. (Now you know why the nickname “fungal acne” has stuck.) The two conditions have entirely different causes and require entirely different treatments. But pityrosporum folliculitis is usually easy to treat with a few over-the-counter products.
Fungal acne isn’t acne, and it isn’t a medical term, let’s get that straight right off the bat.
“Fungal acne is a misnomer,” says Dr. Joyce Imahiyerobo-Ip, a board-certified dermatologist and the CEO of Vibrant Dermatology in Greater Boston, MA. “In dermatology, fungal acne isn't a true diagnosis.”
“Fungal acne” is the colloquial nickname for a fungal infection called pityrosporum folliculitis, which is caused by an overgrowth of Malassezia, a category of fungus, made up of yeasts, that everyone has on their skin. That extra yeast clogs the hair follicles (AKA pores) and makes whitehead-looking bumps that get mistaken for acne pimples. If untreated, the infection might spread, which is ironic, because the name “fungal acne” has done the same thing on social media—the term is everywhere, and dermatologists are trying to set the record straight.
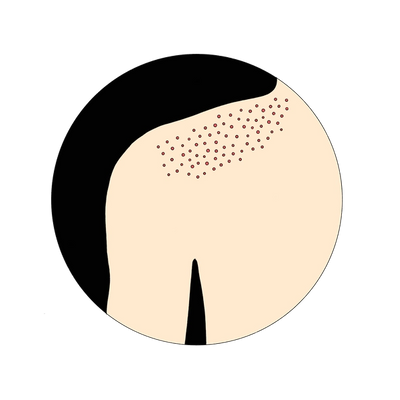
Pityrosporum folliculitis looks like acne, hence the nickname, but it has nothing to do with hormones or oil-and-bacteria clogged pores. Instead, it’s often caused by moisture that’s getting trapped on the skin, maybe from workout gear or other clingy clothing. Unlike acne, fungal acne will look uniform; all the bumps will be around the same size.
It usually presents on the body skin, like the chest and shoulders, but rarely on the face.
—notes Dr. Imahiyerobo-Ip.
Fungal acne (pityrosporum folliculitis) can vary from person to person. One person might get a small patch of that goes away and never comes back, but another person might have a large patch that dissipates and then returns after a few days, months, or even years.
“I find it to be more common in athletes and those who work out a lot,” says Dr. Imahiyerobo-Ip. “It can occur when you wear tight, occlusive clothing or fail to shower right after an intense workout. That said, some people are more prone to yeast than others just based on their intrinsic body chemistry.”
Talk to a dermatologist to diagnose what kind of skin infection you’re dealing with—it might be eczema and not fungal-related at all—and they’ll help formulate a personalized treatment plan for you.
What causes fungal acne (pityrosporum folliculitis)?
Humans have tiny organisms living on the skin at all times—thankfully even the most magnified vanity mirror can’t see them. Two of those microorganisms are fungi and bacteria. Normally, they exist harmoniously, keeping the skin healthy and nourished. However, this natural balance can be thrown off for a number of reasons. When that happens, it can lead to an infection like fungal acne.1
Fungal acne (known medically as pityrosporum folliculitis) is caused by an overgrowth of yeast on the skin—yeast is a type of fungi. That excess yeast clogs the hair follicles and looks like a breakout of pimple-like bumps. (Fungal acne is also called Malassezia folliculitis; Malassezia refers to fungus on the skin, folliculitis refers to an infection of hair follicles.)2
“I explain it to patients as folliculitis,” says Dr. Joyce Imahiyerobo-Ip, a board-certified dermatologist and the CEO of Vibrant Dermatology in Greater Boston, MA. “Folliculitis refers to inflammation of the hair follicles, which can present as pus-filled bumps, or monomorphic papules on the trunk or face (rarely).” (Papules = solid, raised pimples.) “Folliculitis can be caused by many things,” she adds, “In the case of fungal acne, it’s caused by a yeast that is overgrowing on the skin and causing inflammation.” So while fungal acne can cause folliculitis, not all folliculitis is fungal acne.
But where did this excess yeast come from? Yeast grows in warm, humid environments, so if you’re a lifeguard at a Houston water park, watch out. Fungal acne is often caused by moisture trapped on the skin (think: sweaty workout clothes you haven’t changed out of in hours, or wearing a face mask at work all day). It can also be caused by medication. Then again, the yeast overgrowth could also be seemingly random. Skin infections can be like that. It’s maddening. But it’s also treatable. More on that [here].
Fungal Acne Caused by Moisture, Heat, and Darkness
Fungus on the body, like fungi in nature, grows best in warm, dark, and damp environments. Areas of the body that are sweaty and dark, like the feet, groin, and skin under the breasts, are common places for fungal growth. Fungal infections in those areas may go by different names—jock itch, athlete’s foot, intertrigo—but like fungal acne on the shoulders or back, the cause is the same: an excess growth of yeast on the skin.
Tight-fitting clothing, like workout gear, can create dark and humid areas on the body that trap moisture. That’s a known culprit for fungal acne, though not the only one. Changing as quickly as possible out of sweaty gym clothes, a swimsuit, or bringing clothes to change into after biking to work, is a way to avoid a possible fungal infection. Showering after those sweaty activities, and thoroughly drying off, helps even more.
But generally living in a hot and humid climate can increase the likelihood of fungal acne. In those instances, wearing loose-fitting clothing to allow for better airflow—anything to keep sweat from getting trapped on the skin—will help combat fungal growth.
Immunosuppression
The body’s main defense against fungal infections is the immune system. It actively works to combat foreign threats before they lead to infections or illness. So those with immunodeficiency disorders, like AIDS patients, may be more susceptible to fungal infections, as they are with bacterial infections or viruses.
Very generally speaking, maintaining a healthy diet and lifestyle to promote the health of the immune system can be a small way to support the body’s reaction to a flare-up of fungal acne. But admittedly, it’s harder for most people to know if you’re in control over your immune system than it is to make sure you’re not sitting around in sweaty gym clothes. A doctor will best help you figure out the cause and treatment plan for a fungal infection.
Certain Medications
Certain medications can contribute to fungal acne. Normally, bacteria on the skin is on the defense against fungi growing out of control. So antibiotic medications, which are taken to treat bacterial infections, can also eliminate the bacteria on the skin that was preventing fungal spread.
If antibiotic medications might be causing your fungal acne infection, it’s important to talk to a dermatologist or primary care doctor to discuss the best way to treat it.
How do you treat fungal acne?
Acne-specific cleansers, creams, and spot treatments won’t do anything against fungal acne. That’s usually a tip-off that a breakout might be a fungal infection and not acne-acne. In some cases, those acne creams could even make fungal acne worse. The priority for treating fungal acne is to restore the natural balance between yeast and other substances on the skin. This can be done several ways, starting with topical treatments like antifungal creams and dandruff shampoos, and progress to oral medication, as well as changing up a bad hygiene habit, wearing looser clothing, or using skin-drying powders.
Over-the-Counter Antifungals and Steroid Creams
There’s a variety of antifungal creams, shampoos, ointments, and clearing sprays available that can be purchased without a doctor’s prescription at any drugstore or supermarket. These are often the most successful way to treat fungal acne (pityrosporum folliculitis).
A treatment plan for Dr. Joyce Imahiyerobo-Ip, a board-certified dermatologist and the CEO of Vibrant Dermatology in Greater Boston, MA, might look something like this:
“Commonly, I prescribe a medicated anti-yeast shampoo. This is applied to the affected areas, left on for 10 minutes, and washed off. The treatment plan usually lasts for two weeks to a month (if severe). If the yeast is unresponsive, I may add anti-yeast pills. If it’s on the face, there are certain acne medications like benzoyl peroxide and sulfur-based medications that may help improve it.”
Common antifungal creams contain clotrimazole, tolnaftate, econazole nitrate, or terbinafine hydrochloride. Antifungal dandruff shampoos, containing selenium sulfide or zinc pyrithione, can be used as body washes to treat fungal acne, as Dr. Imahiyerobo-Ip suggests.
Look for ointments that say “antifungal” because they probably won’t say “fungal acne” on the container (since that’s the colloquial term for it, it’s not accurate—it’s not acne!). Ointments for athlete’s foot, jock itch, dandruff, or other fungal infections could all work for fungal acne.3 To treat redness and itchiness, hydrocortisone or trimazole cream can help, which are available both over-the-counter and in stronger prescription creams.
As always, there are many treatment routes and talking to a doctor will help narrow down the path that’s best for your case.
Treating Fungal Acne and Dandruff Shampoo
Dermatologists often recommend dandruff shampoo to treat fungal acne on the body. Why? “They’re just antifungal shampoos,” says Dr. Caren Campbell, a board-certified dermatologist in San Francisco, CA. “Dandruff is seborrheic dermatitis, which is caused by malassezia yeast”—the same type of yeast that’s causing pityrosporum folliculitis, which we casually call fungal acne.
Those dandruff shampoos (or scalp treatments and scrubs) typically contain selenium sulfide (like Selsun Blue), zinc pyrithione (classic Head and Shoulders), or ketoconazole (Nizoral), which are all antifungal medications. A stronger version of ketoconazole 2% shampoo is only available with a prescription.
The typical instructions for those shampoos are to apply it to the area with the fungal infection, whether it’s on the body or face, and leave it on for 5-10 minutes, then rinse off. Depending on the strength of the shampoo, it might only be safe to use once or twice a week (refer to the product instructions or double-check with your dermatologist).
As with any skincare treatment, it might take several weeks to see results. And if the shampoo isn’t making a difference, you might need oral medication or prescription ointments in combination with the shampoo, but a dermatologist will know what’s best for your situation.
Get Out of Sweaty Clothes
Fungus grows in wet, warm, and dark locations, whether it’s a sweaty pocket of skin trapped by tight bike shorts, a bra, bathing suit, or sweatband (do people still wear those?). Oh and regular clothes—fungus isn’t too picky. Eliminating that environment on the skin will help keep fungal acne at bay, and since exercising naked isn’t really an option, changing as quickly as possible out of sweaty clothes is the next best bet.
Showering is also important for washing off excess yeast, hopefully before it gets a chance to clog the pores. If you’re working out and not showering afterward, or showering a few hours later, you may be susceptible to fungal infections like fungal acne. Changing up that routine may be a crucial part of your treatment plan.
For those prone to fungal acne flare-ups, showering with antifungal soaps and sprays is a proven effective treatment against current and future fungal infections.
If you or your dermatologist suspect your fungal acne is linked to sweaty situations, establish a new habit as needed: showering and changing in the gym locker room instead of at home, or changing clothes at the end of a long day of work.
Get Really Dry
It might sound obvious, but making sure to dry off entirely after getting out of the shower, bath, or pool will help avoid creating fungus breeding grounds. “You want to keep the area [that’s susceptible to fungal infection] dry,” says Dr. Caren Campbell. Taking away the source of any moisture is the goal.
Certain areas of the skin that might be easy to ignore, or hard to reach, like the center of the back and shoulders, are exactly where you need to show extra attention. So get in there.
(And if for whatever reason you can’t shower after a sweat session, it’s better to dry off as best you can and change into dry clothes, rather than go out for post-soccer match beers in your damp uniform, which, let’s face it, might not smell great either.)
Sometimes moisture on the body is easier to control (towel off!), other times it may feel impossible. Like sweat. If your job is outdoors, and sweating all day is inevitable, there are options like Zeosorb, an over-the-counter drying powder you can sprinkle on before you get dressed for the day. Note that drying powders can be a preventative measure against fungal infection, but they won’t treat infected areas. A doctor can help create a plan that treats and prevents any infections you’re experiencing, based on your skin, body, and your specific circumstances.
Prescription Medication
Fungal acne can be treated with stronger prescription ointments, creams, and prescription oral medications, especially if you tried over-the-counter antifungal creams that didn’t work. See a doctor or dermatologist to diagnose your infection and determine if it needs prescription treatments.
Mass Index Recommends:

Soft Services
Clearing Clay
$28
8 oz
maximum strength
10% sulfur wash, mask, and spot treatment that gently exfoliates dead skin cells, allowing anti-acne, anti-breakout, anti-discoloration, and soothing ingredients to penetrate.

Malezia
Acne Treatment Gel
$11.50
1.7 fl oz
topical antiseptic
Powerful body acne-fighting topical gel with 2.5% benzoyl peroxide that’s been micronized (reduced particle size) to be gentler and less drying.

Soft Services
Clearing Mist
$26
4 fl oz
acne treatment
Salicylic acid treats acne with niacinamide for hyperpigmentation, boosted by zinc PCA and tea tree oil’s antimicrobial and antifungal properties.

Nizoral
Anti-Dandruff Shampoo
$15
7 fl oz
off-label use
A shampoo that uses ketoconazole to treat dandruff, but that can also be used as a body wash (let it sit on the skin for 10 minutes or so) to treat a range of fungal skin infections, like fungal acne (Malassezia folliculitis).
Soft Services works with experts to review the accuracy of our content, but they do not endorse the products we made.
How do you prevent fungal acne?
Fungal acne occurs because of a yeast build-up on the skin; and the yeast can only build up if there’s a dark, moist place for it to grow. That makes treating and preventing it much easier than other more complex skin conditions.
Showering regularly to wash yeast off, and changing out of sweaty clothes as soon as possible to keep it from growing, are two of the easiest and strongest defenses against a fungal acne infection.
For those who are prone to fungal infections, it’s important to continue to use antifungal soaps even after the infection has cleared. While it’s not necessary to use them as often, using these once a week can help keep yeast overgrowth at bay.
The exact skincare regimen for you is just that, uniquely yours. So seeing a dermatologist to guide you on preventing your fungal acne, which might be triggered by a very specific thing (those lucky bike shorts…), will help determine your best course of action. This is especially true if it seems like the fungal acne keeps showing up after several rounds of over-the-counter treatment.
Citations
1Topographical and temporal diversity of the human skin microbiome by Elizabeth A Grice et al. Science.
2Malassezia (Pityrosporum) Folliculitis by Richard M. Rubenstein, MD and Sarah A. Malerich, BS. J Clin Aesthet Dermatol.
3Fungal Diseases Homepage by the Centers for Disease Control and Prevention.
Additional References:
Acne vulgaris, probiotics and the gut-brain-skin axis - back to the future? by Whitney P Bowe and Alan C Logan. Gut Pathog.
Fungal infections by Carol A Kauffman. Proc Am Thorac Soc.
Get Updates
There’s more to come.
Sign up to receive periodical updates on Mass Index, and to be the first to know when Soft Services launches new products. (If we don’t have any updates, we won’t email you.)




















