Keratosis Pilaris
ker-a-tos-is -pi-ˈler-əsSmall, harmless bumps that occur when hardened plugs of dead skin cells form around the hair follicle, especially when skin is dry.
Also Called
KP, chicken skin, bumpy arms, permanent goose bumps
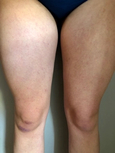
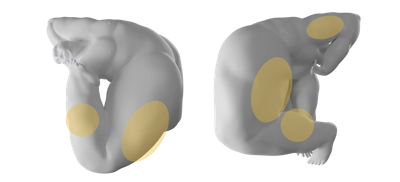
Frequently Found On
Back of upper arms, outer thighs, back of thighs, outer calves
Looks Like
View GalleryWhat is Keratosis Pilaris?
Keratosis pilaris is a very common skin condition—harmless small bumps—that shows up in 40 percent1 of adults. That number is probably even higher because many people who have KP might not notice the small patch of bumps on the back of their upper arms, or they might choose to simply ignore it. Some people call it “chicken skin,” because it shows up pink/red on lighter skin tones, but it can appear purple or dark brown on darker skin tones (usually it’s a few shades darker than your skin tone).

One of many forms of hyperkeratosis, keratosis pilaris is bumps made of keratin, a protein produced in the top layer of the skin, that isn’t shedding properly and is clogging the hair follicles. Think of them as skin-bumps-made-of-dead-skin-cells. Unlike pimples, you can’t “pop” the bumps, and scratching or picking them can cause redness, irritation, lesions, and scarring.
There’s nothing dangerous or contagious about KP, so the medical community considers it a cosmetic issue that mainly affects the appearance of the skin, and not a big deal. As a result it’s hard and frankly frustrating to find definitive answers to a lot of questions about KP; it just hasn’t been the subject of many medical studies. What doctors do know is that it tends to be genetic and is often associated with people who have dry skin. It commonly shows up in childhood, but it can also appear in adulthood, and during pregnancy; it has associations with obesity, diabetes, as well as malnutrition. While it isn’t completely curable, it’s usually treatable with a change in skincare routine. The most important thing to recognize is that it’s not something dangerous to your overall health, it’s incredibly common, and you just have to be patient with treatment, but it is treatable.
You might moisturize three times a day, experiment with exfoliants, or ignore it and get on with your life. As with all things skincare, there is no one-size-fits-all treatment. A big part of the KP journey is finding out the best treatment for your skin. There are a few subtypes of KP that are more severe and require different treatment, so if you’re unsure about what the bumps on your skin are, there is never harm in seeking actual medical advice. Thanks to the increase of telehealth appointments due to coronavirus, you don’t even need to leave the comfort of your couch—many common dermatologic conditions can be identified through remote video or photo consultations with a doctor.
Often confused with:
—goose bumps - Occur when hair follicles perk up when experiencing stress, creating a fine, bumpy texture on skin.
—ichthyosis vulgaris - A scaly skin texture that results from a chronic buildup of keratin on the surface.
—follicular eczema - Cracked, weepy, and/or scaly skin resulting from atopic dermatitis reactions that take place in the hair follicles.
What causes Keratosis Pilaris?
Studies have shown that keratosis pilaris is often genetic. It’s also common in people with sensitive skin who might have a history of eczema (aka “atopic dermatitis”), notes Dr. Caroline Chang of the Rhode Island Dermatology Institute. She describes it to her patients as: “Instead of a hair growing out of your skin, a small hard piece of skin (a keratin plug) forms over your hair follicle.” That piece of skin is what feels bumpy.
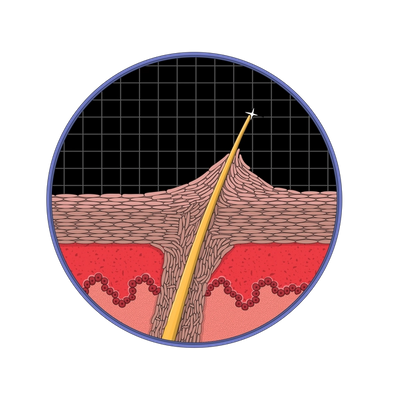
There hasn’t been enough research to know exactly why the buildup of keratin in the skin occurs. Most doctors just refer to the “abnormal keratinization” of the skin cells: a random thing that happens sometimes because bodies aren’t perfect. Another theory relates it to the hair shaft, because samples from a group of people with KP found a hair still coiled up under the skin, causing doctors to hypothesize that those coiled hairs throw the skin’s keratin functioning out of whack. And finally, studies have found that patients with KP tend to show an absence of sebaceous glands, which are minuscule glands on the skin that secrete oil to self-moisturize the skin—exactly what Dr. Chang was talking about when she mentioned patients with KP tending to have other dry skin issues. It’s all related.
How do you treat Keratosis Pilaris?
Treatment of keratosis pilaris requires patience and consistency. It all starts with gentle skincare. Avoid long hot showers, use gentle cleansers, and moisturize, because often KP gets worse when your skin is dry. In cleansers and moisturizers, look for formulas with “keratolytic agents,” meaning ingredients that work by softening, and slowly exfoliating the keratin plugs that are clogging the pores—the bumps. These include lactic acid and salicylic acid, which both have positive clinical results for treating KP.2 Others include alpha hydroxy acid, glycolic acid, and urea. (If you’ve heard of “chemical exfoliants,” that’s what these are.)
Depending on how dry the skin is, a simple treatment plan might begin with moisturizing two-to-three times a day, and assessing whether the bumps have faded in the next two weeks. For more severe cases, a dermatologist can prescribe a vitamin A derivative in the form of topical retinoids (these could be “retinol,” “tretinoin,” or “tazarotene”) which can help address the bumps, but they can also dry the skin, while steroid creams can help with underlying inflammation and redness but are for short-term use only. New targeted laser treatments are also available that can potentially clear clogged pores and reduce inflammation, but dermatologists usually recommend over-the-counter skincare treatment options first (i.e. lotions, cleansers, etc. that you can buy without a prescription).
It’s important to remember that, as with anything skin-related, everyone’s treatment might be different, and some are fine with ignoring the bumps altogether. There’s not a one-size-fits-all answer, and treatment for KP is usually a little bit slow going. It might take weeks for bumps to fade, and sometimes they fade for no reason at all.
Mass Index Recommends:

Soft Services
Smoothing Solution
$30
3.3 fl oz
fragrance-free
This is a leave-on chemical exfoliant containing 10% AHA to dissolve build-up of dead skin cells and soothing ingredients to calm visible irritation.

First Aid Beauty
KP Bump Eraser Body Scrub
$28
8 oz
pumice exfoliant
Body scrub that improves the appearance of keratosis pilaris skin bumps with exfoliating pumice beads, glycolic and lactic acids, and soothing Vitamin E.

Soft Services
Buffing Bar
$30
net wt 3.75 oz (2)
fragrance-free
This is a set of two physical exfoliating bricks for body skin made of fine sanding crystals compressed within a moisturizing, soothing base.

Skinfix
Resurface+ Glycolic Renewing Scrub
$30
8 oz
pre-shower scrub
Exfoliant scrub that’s applied a few minutes before showering to let the chemical exfoliants—glycolic and lactic acids—penetrate the skin to clear away dead skin, smoothing keratosis pilaris skin bumps.
Soft Services works with experts to review the accuracy of our content, but they do not endorse the products we made.
How do you prevent Keratosis Pilaris?
There is no known way to prevent keratosis pilaris, but you can maintain a skincare regimen to continually treat the underlying condition. Keep moisturizing regularly with a product that includes a keratolytic agent, those ingredients that soften the skin like urea, lactic acid, alpha hydroxy acid, glycolic acid, or salicylic acid. Certain environmental factors can dry skin and worsen KP, so make note of dry air (especially in winter months), and consider a humidifier if your skin tends to become tight, itchy, and flaky. Taking long hot showers and swimming in chlorinated pools can also dry out and irritate the skin, setting off KP. Certain clothing exacerbates KP, and any fabric that can rub and irritate skin, like wool, can contribute to worsening KP, as well as tight synthetic fabrics. Similarly, avoid physical exfoliators that feel uncomfortable and inflame skin, like a loofah made of sandpaper.
Citations
1 Skin diseases associated with atopic dermatitis by Clin Dermatol. National Library of Medicine.
2 Epidermal Permeability Barrier in the Treatment of Keratosis Pilaris by Tanawatt Kootiratrakarn. Dermatology Research and Practice.
Additional References:
High body mass index, dry scaly leg skin and atopic conditions are highly associated with keratosis pilaris by G Yosipovitch 1, B Mevorah, J Mashiach, Y H Chan, M David. National Library of Medicine.
Ichthyosis vulgaris by Mayo Clinic Staff.
Keratosis Pilaris by Keith B. Pennycook and Tess A. McCready. National Center for Biotechnology Information, U.S. National Library of Medicine.
Keratosis Pilaris and its Subtypes: Associations, New Molecular and Pharmacologic Etiologies, and Therapeutic Options by Jason F. Wang and Seth J. Orlow. National Library of Medicine.
Keratosis Pilaris: Diagnosis and Treatment by the American Academy of Dermatology Association.
Keratosis Pilaris Rubra A Common but Underrecognized Condition by Ann L. Marqueling, Amy E. Gilliam, Julie Prendiville, et al. Jama Dermatology.
Get Updates
There’s more to come.
Sign up to receive periodical updates on Mass Index, and to be the first to know when Soft Services launches new products. (If we don’t have any updates, we won’t email you.)