Discoloration
duh · skuh · lr · ei · shnDiscoloration indicates an area of skin, maybe a dot or a patch, that's darker or lighter than its base tone.
Also Called
Hyperpigmention, hypopigmentation, scar, freckles, melasma
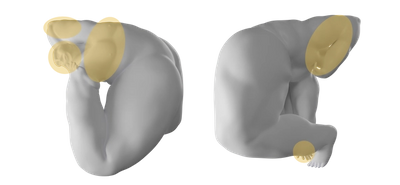
Frequently Found On
Neck, chest, hands, arms
What are the different types of skin discoloration?
Skin discoloration is a big, blanket term for any kind of change in skin color, from a sunburn to vitiligo. Even the dark streak left from burning your forearm on the oven door is considered skin discoloration. And freckles, too. "I see skin discoloration every single day,” says Dr. William Kwan, a board-certified dermatologist and expert in skin of color in San Francisco, CA. And while most skin pigment issues are harmless, that doesn’t mean you should ignore that new spot on your arm. “One dark spot could be a melanoma for all we know,” he says. “So I would much rather see a thousand patients that come in with nothing [beyond a pigmentary issue], than to sit on something for too long.”
Some patients with skin discoloration also have psychological stressors, like self-consciousness and embarrassment, because of it.1 Many skin discolorations, like acne hyperpigmentation (acne scars) are harmless to the body, so they don’t need to be treated—but they can be. There are several ways to treat discoloration, and while treatment can take time (weeks to months to years, depending on the deepness of the pigment), there are options worth seeking out, from lightening creams to lasers.
So yes, you should see a dermatologist if a dark spot concerns you to check it out for signs of melanoma. But even if the look of it bothers you, there’s probably something you can do about it, and that’s a valid reason for visiting a dermatologist too.
Hypopigmentation
Hypopigmentation means there’s a change in skin color to a tone lighter than the base skin color because the body isn’t producing as much melanin. Hypopigmentation could be all over the body, or in just a few spots, like a patch of skin healing from a bit of eczema. Vitiligo and albinism are examples of skin experiencing hypopigmentation; in the case of albinism, the body isn’t producing any melanin at all. Certain skin traumas—that burn from the oven door—can also cause hypopigmentation. Because hypopigmentation is usually associated with other internal medical conditions, it isn’t as common as hyperpigmentation, when the skin darkens, often because of outside injury to the skin like the sun (which has its rays set out for all of us).
Hyperpigmentation
Hyperpigmentation is when the skin darkens, and it can happen for a wide range of reasons, “typically in response to some type of injury to the skin,” says Dr. Kwan, and these are what doctors call “post-inflammatory hyperpigmentation,” he notes. “It could be inflammation like eczema. It could be an acne lesion, like a pimple. It could be a burn. It could be a scrape. Any of those things can potentially hyperpigment the skin.” Skin of color, which contains more melanin to begin with, is more likely to hyperpigment than paler skin;2 and postinflammatory hyperpigmentation is one of the most common reasons patients with darker skin tones visit a dermatologist.3
Some hyperpigmentation is associated with hormonal changes—as in the case of melasma, more on that later—and other medical conditions, including cancer. But generally hyperpigmentation fades over time, from months to years. Depending on how much it bothers you, you can treat it with lightening creams and/or laser treatments, or ignore it. Always talk to your dermatologist about your options.
Melasma
Melasma is hyperpigmentation that typically shows up as brown or dark, splotchy patches on the face, cheeks, lips, forehead, and sometimes neck. It can be triggered by a hormonal change, like birth control medication, pregnancy, and hormone replacement medications—but it can be genetic, and triggered by sun and heat as well. The exact cause of melasma isn’t medically certain, but studies show that whatever the cause, it becomes worse in the sun.4 Melasma is common in women, but men can experience it too. “I’m one of those men that actually got it,” says Dr. Kwan. “And I probably got it from sun exposure.” He’s had patients who had melasma flare after spending time in a sauna, or after doing Bikram yoga, and even a baker who spends their days in front of a hot oven.
While pregnancy-related melasma typically ends after giving birth, for others, melasma can be a lifelong condition. And because melasma is so tied up with sun exposure, treating it calls for a lifestyle change: “I tell my melasma patients, ‘if you truly want to get your melasma under control, you really have to think of those places where you might be getting sun or exposure to heat.’”—and avoid them—says Dr. Kwan. That might mean wearing a floppy hat and sun-protective clothing at the beach, or canceling the Bikram membership. “Usually, melasma is chronic,” he adds, “and patients are constantly treating it whenever it flares.”
Other treatments, like lightening creams, intense pulsed light, and various laser treatments, can lighten areas of melasma, but these don’t “cure” it completely, and some patients report their melasma returning.5
Melasma is also called “the mask of pregnancy” and is the same thing as “chloasma,” but doctors use the term melasma more often.
Chloasma
Chloasma is lesser-used term for melasma; technically, they’re the same thing.
Acanthosis Nigricans
Acanthosis nigricans is a skin condition in which the skin darkens and takes on a velvety texture in folds and creases of skin, usually in the neck, arm, and groin area. It’s often associated with obesity, diabetes, or weight gain, but it might present in patients with cancer, or as a reaction to certain medications. “It’s not necessarily hyperpigmentation,” notes Dr. Kwan, “It’s actually a velvety texture to the skin that does look darker, but it’s more involved than just pigmentation. There are epidermal changes.” Acanthosis nigricans isn’t harmful, but it could be a sign of a yet-undiagnosed condition like diabetes, so it’s important to have it checked out by your doctor.
What causes discoloration?
Skin discoloration can be caused from hormonal changes to sun exposure to reactions from certain products and medications, and as a result of some medical conditions.
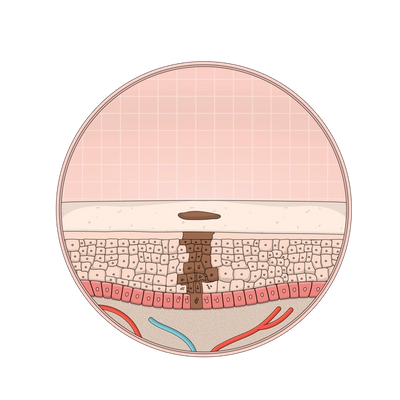
But it all has to do with melanin, a pigment produced in the body that gives skin its range of color (darker skin tones have more melanin than paler tones). On a biological level, what causes the skin to change color is an increase or decrease in melanin, but why exactly the melanin increases isn’t always clear.
It is known that the sun is a major culprit for many varieties of skin discoloration. Evidence suggests that melanin exists to protect skin from the sun; as a defense mechanism, the body produces more melanin when it’s exposed to the sun, which is why skin tans, and sunburns (leading to possible skin cancer—melanin isn’t always your friend).3
Hyperpigmentation, whether from sun spots, melasma, or acne/eczema scars, is made worse from sun exposure. But melanin levels in the skin can be affected by medications or hormone changes that interfere with the body’s production of melanin too (think of how hormone levels change too); there are chemical reactions happening underneath our skin that can show themselves as spots here and there. Even a bug bite from last summer can transform into a long-lasting spot on your ankle. If you’re unsure about any discoloration on your skin, though, have a dermatologist check it out before writing it off as an old bug bite.
How do you treat skin discolorations?
Treatment for skin discoloration depends on the root cause of it. For example, someone can use lightening creams on patches of melasma, but it’s important that they stay out of the sun too.
Someone with acanthosis nigricans might use a chemical exfoliant to soften the hardened skin, but that won’t treat the condition itself, which might require medication, weight loss, insulin management, or other lifestyle changes.
One of the most common ingredients to treat hyperpigmentation—for melasma, sun spots, “age spots” (technically not a real thing), or acne scars—is hydroquinone which inhibits the skin from producing more melanin, though you'll need to see a derm to get a prescription for it. “I think all of us dermatologists would write [a prescription] for hydroquinone right off the bat for hyperpigmentation,” says Dr. Kwan. Hydroquinone could have risky long-term effects that haven’t been definitely studied yet,6 but there are other lightening creams available over-the-counter, such as kojic acid, azelaic acid, tranexamic acid, retinoids, alpha-arbutin, soy, licorice extract, and Vitamin C, among others.7
Lasers and peels may not lighten the skin any more than topical creams. They can, but I always tell my patients that they may not do anything. That’s the worst case scenario.
—says explains Dr. Kwan, a board-certified dermatologist and the founder of Kwan Dermatology in San Francisco, CA.
Another option for lightening the skin is targeted laser treatment, of which there are a few varieties. Some patients want to treat the skin discoloration as aggressively and quickly as possible by going straight to the lasers, but “it’s not one or the other,” with lasers and lightening creams, notes Dr. Kwan. For people with skin pigment issues (not skin discoloration due to a medical condition), he only treats with lasers once the patient is on some type of topical lightening agent first since those will sink into the skin and target melanin production itself—lasers will aim to physically zap away the discoloration. “Lasers and peels may not lighten the skin any more than topical creams. They can, but I always tell my patients that they may not do anything. That’s the worst case scenario.” It’s important to take your treatment course of action with the guidance of a doctor—overdoing it on certain lightening agents and chemical peels, and laser therapies can risk making the hyperpigmentation worse.
Mass Index Recommends:

Dr. Dennis Gross
Alpha Beta® Exfoliating Body Treatment
$58
8 pk
exfoliating towelette
Single-use towelettes soaked with multitasking liquid exfoliants (AHAs and BHAs) that cause skin cell turnover and can treat skin discoloration with long-term use.

Soft Services
Smoothing Solution
$30
3.3 fl oz
fragrance-free
This is a leave-on chemical exfoliant containing 10% AHA to dissolve build-up of dead skin cells and soothing ingredients to calm visible irritation.
Soft Services works with experts to review the accuracy of our content, but they do not endorse the products we made.
How do you prevent skin discolorations?
If you notice freckles appear after you spend time in the sun, or if you’ve had patches of melasma after a week at the beach, you can prevent it from flaring by avoiding that sun exposure altogether. But if that’s too extreme (understandable, the beach is the beach), wearing as much sun protective clothing on top of your full-spectrum SPF can keep melasma at bay, depending on the person. (Though you’ve definitely heard this before: sunscreen should be a regular part of all skincare routines, most notably because it helps prevent skin cancer.)
To prevent hyperpigmentation from acne, treating the acne first will decrease the likelihood of those subsequent spots. Also known as “post-inflammatory hyperpigmentation,” the darkened spots occur because the acne acts as a stressor that triggers melanin production. What causes more inflammation? Picking, popping, and prodding the acne—so avoid this at all costs. The same goes for hyperpigmentation from atopic dermatitis (eczema) or psoriasis, each requires its own treatment to help prevent things like scratching that leads to scarring that may hyper-or hypo-pigment the skin. Other skin discolorations might be genetic or just unavoidable, like a random burn, or conditions like vitiligo, which is an auto-immune disorder.
Citations
1Psychosocial impact of acne and postinflammatory hyperpigmentation by Katlein França and Jonette Keri. Anais Brasileiros de Dermatologia.
2Postinflammatory Hyperpigmentation by Erica C. Davis, MD and Valerie D. Callender, MD. The Journal of Clinical and Aesthetic Dermatology.
3Clinical and Biological Characterization of Skin Pigmentation Diversity and Its Consequences on UV Impact by Sandra Del Bino, Christine Duval, and Françoise Bernerd. International Journal of Molecular Sciences.
4Melasma: a clinical and epidemiological review by Ana Carolina Handel, Luciane Donida Bartoli Miot, and Hélio Amante Miot. Anais Brasileiros de Dermatologia.
5A review of laser and light therapy in melasma by M.K. Trivedi, BS, BA, et al. International Journal of Women's Dermatology.
6Hydroquinone and its analogues in dermatology - a potential health risk by W Westerhof and T J Kooyers.J Cosmet Dermatol.
7Are Natural Ingredients Effective in the Management of Hyperpigmentation? A Systematic Review by Jasmine C. Hollinger, MD, Kunal Angra, MD, and Rebat M. Halder, MD. The Journal of Clinical and Aesthetic Dermatology.
Additional References:
The Protective Role of Melanin Against UV Damage in Human Skin by Michaela Brenner and Vincent J. Hearing. Photochem Photobiol.
Acanthosis nigricans: To be or not to be afraid by Maria-Linda Popa, Adrian Claudiu Popa, et al. Oncology Letters.
Get Updates
There’s more to come.
Sign up to receive periodical updates on Mass Index, and to be the first to know when Soft Services launches new products. (If we don’t have any updates, we won’t email you.)





















